Prostatitis is one of the most common yet misunderstood conditions affecting men of all ages. It refers to inflammation of the prostate gland — a small organ located just below the bladder that plays a crucial role in sexual and urinary function. When this gland becomes irritated or infected, the result can be a mix of pain, urinary issues, fatigue, and even emotional stress.
Unlike prostate cancer or benign prostatic hyperplasia (BPH), prostatitis can appear suddenly and affect men well before middle age. While medical treatment is often essential, recovery also depends on lifestyle, stress management, and proactive self-care.
This guide explains the causes, symptoms, and treatment options for prostatitis — along with natural ways to support recovery and protect your prostate health long-term.
Table of Contents
What Is Prostatitis?
Prostatitis means inflammation of the prostate gland. It can be bacterial or non-bacterial, acute or chronic, and may cause both physical pain and urinary disturbances.
Doctors generally classify prostatitis into four categories:
🔹 Acute bacterial prostatitis – caused by bacterial infection, often with fever, chills, or severe pain.
🔹 Chronic bacterial prostatitis – recurring infections that flare up periodically.
🔹 Chronic prostatitis / chronic pelvic pain syndrome (CP/CPPS) – the most common type; symptoms persist but without bacterial infection.
🔹 Asymptomatic inflammatory prostatitis – inflammation detected during tests but without symptoms.
According to the Cleveland Clinic and the National Institutes of Health (NIH), prostatitis is one of the most frequent urological diagnoses among men under 50.
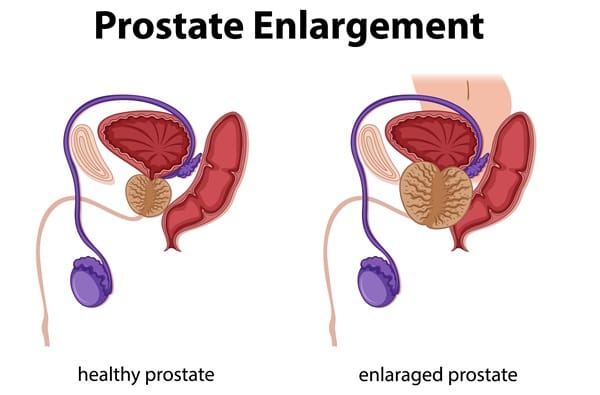
It’s important to differentiate prostatitis from enlarged prostate (BPH) and prostate cancer:
💡 BPH causes urinary blockage but usually not pain.
💡 Cancer often progresses silently.
💡 Prostatitis, by contrast, tends to cause noticeable discomfort and inflammation.
Causes and Risk Factors
The cause of prostatitis depends on the type. Acute and chronic bacterial cases usually stem from urinary tract infections, medical procedures, or bacteria entering the prostate from the urethra.
However, in many men with chronic prostatitis, no infection is found. Instead, the causes may include:
🌿 Pelvic floor muscle tension or nerve dysfunction
🌿 Autoimmune or inflammatory responses
🌿 Prolonged sitting or cycling
🌿 High stress levels
🌿 Dehydration and poor circulation
🌿 Previous pelvic injury or surgery
The NIH notes that chronic pelvic pain syndrome (CPPS) accounts for up to 90% of prostatitis cases — often with no bacterial trigger. Chronic tension and stress can worsen inflammation and discomfort.
The Link Between Lifestyle and Prostatitis
Modern lifestyles play a major role in prostate health. Men who sit for long hours — especially office workers, drivers, or cyclists — may restrict blood flow to the pelvic region, increasing inflammation risk. Poor hydration, smoking, and diets high in sugar and processed foods can also contribute to chronic irritation. On the other hand, regular exercise, mindful posture, and relaxation practices can help protect the prostate and reduce future flare-ups.
Recognizing Prostatitis Symptoms
Symptoms can vary depending on whether the prostatitis is acute or chronic. Common signs include:
✅ Burning or pain during urination
✅ Frequent or urgent urination
✅ Pain in the lower back, groin, perineum, or inner thighs
✅ Discomfort during or after ejaculation
✅ Difficulty starting urination or weak urine flow
✅ Fatigue, fever, or body aches (in acute cases)
In chronic forms, men often experience persistent pelvic pain without fever. The condition can be frustrating — symptoms wax and wane, sometimes lasting for weeks or months.
Diagnosis and Medical Evaluation
Because prostatitis symptoms overlap with other prostate disorders, proper diagnosis is vital. A healthcare provider may perform:
🩺 Digital rectal exam (DRE) to assess prostate tenderness.
🩺 Urine and blood tests to detect infection.
🩺 Prostate secretion or semen analysis for bacteria.
🩺 Ultrasound or MRI if chronic inflammation is suspected.
If you experience fever, severe pain, or urinary retention, seek medical attention promptly — acute bacterial prostatitis can become serious if untreated.

Conventional Prostatitis Treatments
Medical therapy remains the first line of treatment, particularly when infection is present.
💊 Antibiotics
Doctors often prescribe antibiotics such as fluoroquinolones or trimethoprim-sulfamethoxazole. The course may last from two to six weeks, depending on the infection’s severity. According to Healthline, these are effective for bacterial prostatitis, though chronic cases may require longer therapy.
🧘 Alpha-blockers
These medications relax bladder neck muscles and prostate fibers, helping relieve urinary difficulty and pain.
💧 Anti-inflammatory agents
Nonsteroidal anti-inflammatory drugs (NSAIDs) reduce swelling and discomfort.
⚙️ Supportive care
For persistent cases, physiotherapy, biofeedback, or pelvic floor relaxation therapy may help release tension that contributes to chronic pain.
Even with antibiotics, symptoms may linger — this is where combining medical treatment with lifestyle adjustments becomes critical.
Chronic Prostatitis and Pelvic Pain Syndrome
Chronic prostatitis, or chronic pelvic pain syndrome (CPPS), can affect men physically and emotionally. Because infection isn’t always present, treatment focuses on symptom management and quality of life.
Effective strategies include:
- 🌿 Pelvic floor physical therapy to retrain muscles and relieve pressure.
- 🌿 Stress management using mindfulness or breathing exercises.
- 🌿 Regular movement to improve circulation and reduce inflammation.
- 🌿 Heat therapy, such as warm baths or compresses, to soothe discomfort.
When Prostatitis Becomes Chronic
For some men, prostatitis turns into a long-term condition marked by cycles of pain, tension, and fatigue. Experts believe this happens when nerves in the pelvis become hypersensitive after repeated inflammation. Managing this form involves patience and a multi-modal approach — physical therapy, targeted stretching, relaxation, and even acupuncture can help reduce pain and restore mobility. Treatments like biofeedback and mindfulness-based stress reduction (MBSR) have shown promise in easing symptoms and improving coping mechanisms.
For men with long-term pelvic tension, gentle Pelvic Massage and breathing techniques can help restore circulation and ease discomfort.
Natural Remedies and Self-Care for Prostatitis
Many men complement medical treatment with natural remedies to help relieve prostatitis pain and inflammation.
Hydration and diet
💡 Drink plenty of water and limit alcohol, caffeine, and spicy foods — all of which can irritate the bladder and prostate.
💡 Incorporate anti-inflammatory foods like salmon, berries, leafy greens, turmeric, and green tea.
The Cleveland Clinic also recommends avoiding processed foods and staying active to support recovery.
Gentle movement
✅ Avoid sitting for long periods.
✅ Walking or stretching improves pelvic blood flow and reduces pressure.
Heat therapy
🔥 Sitz baths or warm compresses can help soothe pelvic pain and promote relaxation.
Stress reduction
🌿 Chronic stress tightens pelvic muscles and can exacerbate pain. Daily relaxation practices, meditation, or yoga can make a significant difference.
Natural supplements
💊 Some men find relief with quercetin, saw palmetto, or pollen extracts, though research remains mixed. Always consult your doctor before starting supplements.
Diet and Exercise for Prostate Health
Eating a Mediterranean-style diet rich in omega-3 fats, whole grains, and antioxidants can reduce inflammation and support hormonal balance. Regular moderate exercise — such as swimming, yoga, or brisk walking — boosts circulation and helps regulate stress hormones that affect prostate function.
Many also find value in targeted self-massage. Our guide on Male Massage Techniques offers safe, practical ways to ease tension and boost circulation.

Prostate Massage and Circulation
Improving blood flow to the prostate can help clear congestion, deliver nutrients, and relieve pressure. Prostate massage — performed gently and correctly — has been explored as a way to reduce inflammation and support healing.
While not suitable for acute infection, it may assist with fluid drainage, pain relief, and even enhance sexual wellness by improving prostate orgasms and muscle relaxation.
🔗 Curious about how external prostate massage can support recovery?
Read our complete guide: External Prostate Massage: A Complete Guide
Preventing Recurrence and Supporting Prostate Health
Once symptoms improve, maintaining a healthy lifestyle can help prevent recurrence:
✅ Stay hydrated and urinate regularly.
✅ Avoid prolonged sitting or tight clothing.
✅ Exercise moderately to boost circulation.
✅ Manage stress effectively.
✅ Get enough rest and maintain sexual activity if comfortable — it supports normal prostate function.
✅ Schedule regular checkups for early detection.
Long-Term Prostate Wellness
Men over 40 should schedule annual prostate exams, even if symptoms are mild. Preventive care, early diagnosis, and awareness of changes can significantly reduce complications. Maintaining a healthy weight, limiting alcohol, and balancing blood sugar also protect long-term prostate function.
The Emotional Side of Prostatitis
Chronic prostatitis doesn’t just affect the body — it impacts mental and emotional health too. Constant pain or discomfort can lead to frustration, anxiety, or even depression. Addressing the emotional component is key to lasting recovery.
Men benefit from open communication with partners, therapy, or participation in online support groups where they can share experiences. Practices like deep breathing and mindfulness also help regulate the nervous system, improving pain tolerance and mental clarity. Healing the mind is part of healing the body.
Frequently Asked Questions
1️⃣ What is the fastest way to relieve prostatitis pain?
Warm baths, anti-inflammatory medications, and gentle stretching can provide quick relief. For bacterial cases, antibiotics are essential. Reducing sitting time and using heat packs on the perineum can also ease discomfort.
2️⃣ Does prostate massage help prostatitis?
Acute prostatitis usually resolves within several weeks. Chronic prostatitis or CPPS may take months of combined therapy and self-care before symptoms settle.
3️⃣ How long does prostatitis last?
Acute prostatitis usually resolves within several weeks. Chronic prostatitis or CPPS may take months of combined therapy and self-care before symptoms settle.
4️⃣ Can stress cause prostatitis?
Yes. Chronic stress can tighten pelvic floor muscles and disrupt nerve pathways, contributing to persistent inflammation even without infection.
5️⃣ What foods help reduce prostate inflammation?
Anti-inflammatory foods like salmon, blueberries, tomatoes, leafy greens, and nuts may support prostate health. Limit alcohol, processed foods, and caffeine.
6️⃣ How can I tell if I have prostatitis or an enlarged prostate?
An enlarged prostate (BPH) usually causes urinary blockage but little pain. Prostatitis often causes pelvic or perineal pain. Only a medical evaluation can confirm the difference.

Conclusion
Prostatitis can be frustrating — but recovery is possible. Combining medical treatment with lifestyle care, relaxation, and consistent communication with your healthcare provider can make all the difference.
Every man’s experience with prostatitis is unique. Stay patient, stay informed, and take an active role in your wellbeing.
📚 References
- Cleveland Clinic. Prostatitis: Causes, Symptoms, Diagnosis & Treatment. Accessed 2025.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIH). Prostatitis. Accessed 2025.
- Healthline. Prostatitis: Symptoms, Causes, and Treatment Options. Accessed 2025.
- Cleveland Clinic Health Essentials. What Is Prostatitis and How Is It Treated?. Accessed 2025.
⚠️ Disclaimer:
This article is for informational purposes only and does not constitute medical advice. Always consult with a licensed healthcare provider or certified massage therapist before beginning any new treatment, especially if you have pre-existing health conditions or concerns.